Bonding is a common cosmetic procedure due to its relatively low cost and ease of application. It is often used to reshape or change the color of a tooth and fill in slight spaces between teeth. The composite material used in bonding can be shaped and polished to match all surrounding teeth.
Looking for Teeth Whitening in Glen Rock? Yearning for a bright youthful smile?
Dr. King offers a full range of cosmetic dentistry including professional teeth whitening. Teeth whitening is the #1 requested and performed cosmetic dental procedure. Teeth whitening (sometimes called teeth bleaching) is a procedure that brightens teeth and helps to remove stains and discoloration.
Throughout the day a thin coating of bio film collect on teeth, the bio film can attract stains that can be trapped in the pores of tooth's enamel.
Teeth whitening by a dental professional is key as cavities need to be treated before teeth are whitened. Cavities are problematic because whitening solution can penetrate the cavity allowing decay to reach inner areas of a tooth. People with good dental health may also use a kit to whiten teeth at home. However, in a single office visit, teeth whitening performed by a dental professional will produce brighter results that are more consistent in color across all teeth.
The most common type of home teeth whitening involves placing a gel-like whitening solution, which usually contains hydrogen peroxide, in a tray that resembles a Nightguard or mouth guard. Over-the-counter mouthpieces are unlikely to fit correctly and can cause gum irritation if the whitening agent seeps out. The tray is then placed over the teeth for a certain period of time, anywhere from an hour or two to overnight.
Single visit whitening uses a special light that is able to activate a higher concentration of whitening solution in order to produce quicker and more dramatic results. Our technicians protect your mouth very carefully and the whole process takes around an hour.

Composite fillings are today's modern filling choice. They are made to match your tooth's natural color to make them virtually invisible to notice and are placed onto the tooth by bonding the filling material to the tooth so they do not have the unlikely chance of falling off. Many patients choose to replace their old silver and gold fillings with composite fillings.
Other Benefits:
- Beautiful in appearance
- Completed in a single visit
- Form a strong seal
- Less chance of tooth cracking
A veneer procedure is a popular cosmetic procedure. Porcelain is known as one of the best materials for esthetic dental procedures, because it mimics tooth enamel very closely. Veneers are extremely thin (usually less than 0.5 mm thickness), giving them enamel-like translucency, creating a natural appearance. They are about as thick as a contact lens. There is very little tooth preparation before the veneer application.
Porcelain veneers are attached to your teeth using a dental bonding glue or cement. Although veneers are very thin, once bonded to your teeth they become strong. The process is fast and conservative. First, your teeth are prepared and impressions are sent to a dental laboratory along with the design for your new smile. Veneers may be recommended along with other cosmetic procedures in order to produce optimum results.
The most conservative approach when attempting to replace a missing tooth is a bonded bridge. It is also often referred to as a Marilyn Bridge. An impression of the area is taken and a new tooth referred to as a pontic is formed. Attached to the pontic on either side are abutments or “wings†that will support the pontic. The most common type of Marilyn Bridge uses abutments that are cemented on the backside of the adjoining teeth and hold the pontic in place where the missing tooth used to be. The adjacent teeth may need to be slightly modified to accept the “wings†of the pontic. The advantage of this type of procedure is that you are not having to put full coverage crowns on the adjoining teeth.
If your smile is in need of a makeover, crowns can provide predictable results. Crowns can give an unattractive tooth back its beautiful shape and color. For smaller or worn down teeth, a crown can restore the natural size of the old tooth. A crown can replace either part of or the tooth's entire structure. For procedures requiring only the areas visible from the outside, a veneer may be an alternative option.
Crowns are used to restore a tooth to its natural size, shape and color after a large filling or crack in the tooth has compromised the tooth. Crowns are almost always placed after a root canal treatment because the tooth becomes weak and is likely to fracture. A crown will strengthen and protect what remains of the tooth and will improve your smile. Crowns are often made of all ceramic material and in some cases can be made in a single visit.
In order for the crown to be placed on the tooth, 1-2mm of the tooth must be taken away and an impression must be made of the tooth. If the office has the ability to make crowns in a day, it will be made and placed on your tooth in the same visit, otherwise the impression is sent to a lab and your crown is fabricated there. If you have to wait on your crown, a temporary is placed on your tooth and will be replaced with your crown when it arrives. When the crown is placed on your tooth, sometimes it needs to be adjusted a little to make the proper fit. After it is adjusted it is cemented to your tooth and is a permanent solution.
A bridge may be used to replace a single tooth. A bridge consists of both a false tooth, called a pontic and the anchors (abutment crowns) that support the pontic. The entire structure spans the space vacated by the missing tooth.
Neighboring tooth structure is removed, shaping them to receive an anchor crown. An impression is then taken and sent to a dental lab where they fabricate the bridge.
The structure part of the bridge is created with a strong metal alloy that can handle the anticipated stresses.
Tooth-like porcelain is then fused to the structure. Once the bridge is tested for a correct fit, the anchor crowns are cemented to the neighboring teeth.
An inlay or onlay is a method of repairing a tooth that is somewhere between a filling and a crown. They are used when the tooth is unable to support a filling, but is not damaged to the point that it needs a crown. An inlay is much like a filling but is inserted into the ridges (cusps) of the chewing surface. An onlay is a little more extensive than an inlay and covers multiple cusps of the tooth. Inlays and onlays are commonly made with ceramic or composite materials but can also be made of gold. They are very durable and can last a long time depending on the material used and how well the patient takes care of them with regular brushing, flossing and visits to the dentist.
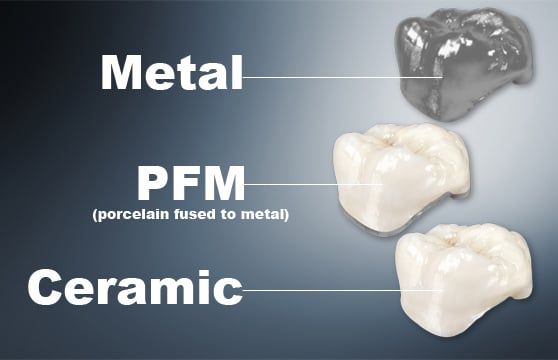
With today’s advances in dentistry, there are several options when choosing a type of crown. The most common crown utilized in dentistry is referred to as a PFM or porcelain-fused to metal crown. For those that have sensitivities to metals or are worried about aesthetics, there are all porcelain crowns or crowns that are composed of a material called composite. There have been several advances in all porcelain crowns and some labs are now utilizing zirconia which is much stronger than a typical porcelain crown. Also, they still are making all metal crowns, which are typically gold, and are usually used on a molar or a back tooth. Of course all of these different options vary in durability, appearance and cost. Please contact our office for any further questions. We would be more than happy to find the crown that is right for you and your situation.

There are four different choices that you have when it comes to filling a cavity.
1. Composite Fillings - Natural tooth colored filling, bonds to the tooth to provide added security.
2. Silver Fillings - Inexpensive and strong amalgam based filling.
3. Gold Fillings - More attractive than silver and provide for a better fit.
4. Porcelain Fillings - Also called inlays; the most attractive and durable of the tooth colored choices.
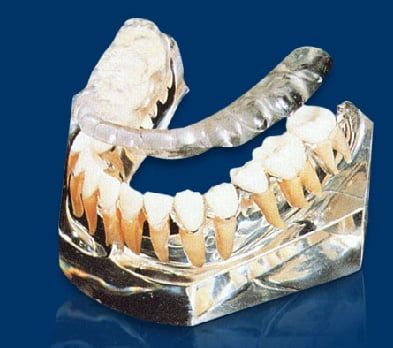
An implant is a titanium "root" which can be placed into the jawbone. Once integrated with your bone, the implant can be used to support a crown, a bridge, or secure a complete denture. Dental implants may be used to eliminate partial plates and dentures. The success rates for dental implants are extremely high which is due in part to the fact that root-form implants are made of a biocompatible material, titanium. Dental implant treatment represents a slightly greater investment than conventional treatment; however, the benefits of implant therapy for most patients outweigh the minor additional cost involved
Implants are a tooth replacement option that involves placing a new "root" into the bone of your jaw. Once this titanium "root" has infused with your bone it can be used to support a crown, bridge, or denture. These implants can also be used to replace partials and other forms of dentures. the success rates for dental implants are extremely high. This is due in part to the fact that root-form implants are made of a biocompatible material, titanium. Because titanium is accepted so well by the human body, it is also used for orthopedic implants, such as hip and knee replacements. Dental Implants have now become the standard for replacing older dentistry and missing teeth because they look and feel like your natural teeth and have a higher success rate than all other forms of tooth replacement. The initial cost is generally higher for an implant over other forms of tooth replacement, but the long term benefits easily outweigh the difference in additional cost. An investment in implant dentistry is an investment in overall health, appearance and well being, as it involves preserving the integrity of facial structures, as well as replacing missing teeth. back to index
Dental implants can last a lifetime, unlike bridges, partials and dentures that may need to be replaced several times. Unlike bridges, partials and dentures, a dental implant replaces the lost tooth root, which will prevent jaw bone resorption that occurs with bridges, partials and dentures. The loss of tooth roots will cause a change of the smile and contours of the face over time. A bridge, once the common single tooth replacement method, requires the alteration of each neighboring healthy tooth, which is cut down and shaped to accept a crown. With a dental implant treatment, there is no compromise to adjacent teeth. The lost root and crown is replaced leaving neighboring healthy teeth in place. Removable partials connect to healthy teeth by hooks. Partials may be removed for cleaning and may need to be replaced often. A partial hooks connected to healthy teeth will create tooth stress and will loosened the healthy teeth over time. Full arch dentures and partials have the added disadvantage of accelerating the bone resorption process, which, among other things, causes the appearance of premature aging. back to index
A single tooth supported by an implant is like turning back the clock of time. The implant replaces the natural tooth root so the jaw bone and supportive gum tissue is as vibrant as ever. Multiple single implants may support single teeth or an implant supported bridge. Dental implants may also support the base for full arch dentures to attach to which provides the look, feel and function of natural teeth. Dental implant treatments is the only tooth replacement solution that prevents jaw bone resorption, which can cause your smile to look unnatural and in some cases, change your facial appearance. The long term esthetics of dental implants are superior to any other treatment option. back to index
If you are missing one or more teeth and in general good health you are a candidate for dental implant treatment. There are a few qualifying factors that need to be addressed:
Overall, there are very few conditions that would keep someone from having implant treatment. Even people who have lost a significant amount of bone can qualify for dental implant treatment; although, an additional procedure(s) to add bone or to create new bone may be necessary. Advances in this type of treatment have made it possible for most people who would not previously have been considered candidates to have successful implant treatment. back to index
Providing your overall health is good there is really no age restriction. The desire to improve your quality of life is frankly a more important consideration than age. It is not unusual for people with dentures to upgrade to implant supported dentures. It provides a renewed self-confidence in their smile and speech and also provides renewed chewing stability, plus brings back foods into their life that were once off limit.back to index
Traditional treatment may take anywhere from several weeks to several months, depending upon the quality of the bone in which the implants are placed. If an additional procedure is required in order to augment the bone, the total treatment time may be between six to nine months. Some implant candidates may qualify for Immediate Load / Immediate Function procedures, also known as "same day implants". back to index
Most implant patients report that the discomfort is far less than they expected and is no more remarkable than having a root canal or like having a tooth extracted. Of course you are anesthetized during the procedure, and although everyone's pain tolerance is different, most patients are very comfortable simply taking over-the-counter analgesics afterward. back to index
Dental implants are designed to be permanent; however, there are a few factors that may contribute to the long term success of dental implant treatment, such as the original quality of the surgical and restorative treatment, proper home care and regular check-up visits to your dentist or dental specialist. Dental implant treatment is one of the most successful procedures in the medical-dental field, with documented success rates over 95%. Dental implants have been around for over 30 years and have closely documented clinical research that demonstrates that dental implants will be successful throughout the lifetime of a patient. By comparison, research also demonstrates that the average tooth supported bridge (conventional dentistry) lasts from 7-10 years and that partials and dentures are functional for approximately 5 years before having to replace the appliance.back to index
Every patient's situation is unique; however, from time-to-time we can use an existing denture by altering the denture to accommodate the necessary denture attachments to fit the implants.
There are several differences.
Although dental implants have become the standard of care, they are more expensive than old tooth replacement methods. They are a better choice for the money; however, some dentists still recommend traditional tooth supported bridges for patients due to their own comfort level, or when patients insist on having the immediate lowest possible fee for tooth replacement. Most dentists today detest the idea of grinding down perfectly healthy teeth to place a traditional bridge, and therefore, will almost always recommend dental implant treatment in these cases.
There are times when it makes sense to extract a tooth and replace it with a dental implant.
Home care for a dental implant single tooth or for a dental implant crown and bridge is cleaned like a natural tooth, with regular brushing, flossing and regularly schedule hygiene appointments as directed by your dentist. Home care is a little more complicated for people who are missing all of their teeth, in that special brushes and floss are often recommended. Permanently fixed implant supported replacement teeth are cleaned like all other bridges. If a surgical specialists who placed the implant(s) is involved, they may want to see you at least once each year in addition to your regular dentist. These visits, combined with proper home care, are essential to the long term success of implant treatment.back to index
The actual cost of dental implant treatment is based on a number of factors, such as the number of missing teeth being replaced, the type of implant supported teeth (treatment option) recommended and whether additional procedures are necessary to achieve the proper esthetic and functional result. The only way to accurately estimate the cost for an individual patient is to have an examination and consultation with your dental specialist. The total fee is usually comparable to other methods of tooth replacement; however, long-term, implant treatment is generally more cost effective than other options, such as bridges, partials and dentures that need to be replaced every 5-10 years. back to index
Dental insurance coverage of implant treatment depends on your individual policy. Dental benefits are determined by the amount an employer is willing to spend on the policy. Generally, dental policies cover basic routine preventive maintenance, basic care and emergencies. Most insurance plans only cover the basics with an annual maximum allowable benefit of $1,000-$1,500. Most insurance plans do not include dental implant coverage; however, often they will pay the same benefit they would cover for the lowest cost alternative treatment option (partials and dentures) and some of the diagnostic records, if a specific request is made for alternative benefits. You should review your dental insurance plan and your medical insurance plan to see the coverages. Medical coverage is very rare and Medicare does not cover implant treatment. All in all, it is best to assume that there is no medical insurance coverage available.back to index
In order to place an implant, a couple of steps must be taken:
1) An incision is made into the gums using very precise measurements, then using a very small drill, the jawbone is given a "tap" that will allow the implant to be placed. After the implant is screwed into place, the gums are closed up and the healing process begins. This process can take approximately three to six months to ensure the implant has fused with the bone and created a sturdy base for the new teeth.
2) When the implant is ready, an abutment is attached to the implant, which allows for a new crown to be placed or a denture to be attached.
Do you have missing teeth? It is critically important to replace missing teeth. Eating and chewing with missing teeth can sabotage your bite and lead to incessant discomfort. Missing teeth can give rise to a mouth rearrangement that often results in facial changes that look decrepit. If a tooth is missing or has been extracted for any reason, a single implant can be used to replace the missing tooth. The implant is placed into the bone of the jaw and acts as the new tooth root. After the bone has healed over the implant an abutment can be placed on the implant and a crown can then be attached. This method of tooth replacement looks and feels like natural teeth.
Multiple tooth implants may be placed if you need or desire to permanently replace an extracted or lost tooth. Titanium implant bases are placed into the jawbone to replace the job of the tooth roots. We allow a period of time to allow for the jawbone to heal over the bases before fitting for a crown. Next, abutments are screwed into the bases of the implants to allow crowns to be attached. Finally, custom fabricated crowns are placed over the abutments and will function like a real tooth.
In many circumstances all of the upper or lower remaining teeth need to be removed due to advanced periodontal disease and/or dental decay. One approach is a full upper or lower plate; however, this treatment modality is not recommended. The treatment of choice is to replace the upper or lower teeth with caps that are in place permanently and supported by dental implants. A common goal of treatment is to have (twelve teeth-caps) supported by eight implants. The four caps that are not supported by the implants are connected to adjacent implant supported caps. With this optimal approach, the maximum amount of bone is preserved.
An MDI mini implant is an implant used to provide better denture stability in patients that cannot handle standard implant surgery, do not have enough bone to support a standard implant or are going from one prosthetic system to another due to continuing therapy.
The top of an MDI implant is shaped like a ball that allows a rubber o-ring to snap in over the ball when the denture is placed onto it. These types of implants can usually be placed in one or two office visits because there is no waiting on the jawbone to heal. In most situations the patient can walk out with their dentures the same day they receive their implants.

1. Eliminates the need to "cut down" the neighboring teeth to make a bridge.
2. Maintains the jawbone structure.
3. Feels and functions like natural teeth.
4. Does not rely on other teeth for support.
5. Replaces partial plates and may be used to secure loose dentures.
6. Cleaned and flossed like a natural tooth.

It is sometimes difficult to get used to your newly placed dentures. They can feel bulky, loose and awkward. In order to make your adjustment period smoother, here are a few guidelines to follow:
- Wear your dentures all the time after you first receive them.
- Never use adhesives on your dentures unless instructed to by your doctor.
- When you go to sleep, remember to always remove your dentures.
- Always brush your dentures after removal and store them in a bowl of water. You can soak your dentures in a denture cleaner as well, but only after you have brushed them.
- If you experience any sore spots, looseness or discomfort please let your doctor know so they can help.
Never try to adjust your dentures on your own, each individual will have a different adjustment period and it will take time for you to become comfortable with your new teeth.
Approximately 40% of your jawbone structure will be gone after wearing your dentures for just six months. You will begin to notice that your dentures aren't fitting the way they used to after a few years of wearing them as well. This is because over the years, the structure of your jawbone becomes unable to support your denture. The same thing happens even if you are wearing a partial denture.
Once the structure of your jawbone is gone, your options for tooth replacement become very limited. Dental implants can stop bone loss and provide your mouth with natural looking teeth before the jawbone structure is completely lost.
A rather comfortable tooth replacement option is a flexible partial denture. These dentures are made from a composite plastic resin and can include a biocompatible metal for superior strength in some cases.
A full arch denture is a removable tooth replacement option for those who need all their teeth replaced. They can be crafted to provide the characteristics (tooth shape and color) the patient desires. Advances have been made in the materials used for dentures and in the way they are designed. If you already have dentures (partial or full arch) you may be experiencing a loose fit or denture slipping. This can lead to gum sores, can affect your chewing and your speech and decrease your confidence when speaking and/or laughing with others. We can help restore your dentures to the correct fit.
This type of denture is made to be placed in the mouth immediately after you have all your natural teeth extracted. This allows you to leave the office without the embarrassment of having no teeth while the gums heal from the extraction. The denture is made to conform to your mouth at the moment impressions were taken. Your gums will change drastically over the next few months and it is possible that the dentures will rub against the gums causing some soreness until the denture is adjusted. Most patients will require a realignment of their denture within the first few months due to the gums shrinking from the extraction of teeth. Another benefit of immediate dentures is the fact that the dentures act as a bandage to the extraction sites which covers the tooth sockets and prevents them from becoming irritated. Just remember, never remove the denture yourself, even for a brief moment unless your dentist has instructed you to. The gums have a tendency to swell when uncovered at first and if you are without your dentures for a little while they may never go back in.
An over denture fits on-top of natural teeth or dental implants. Many patients suffer with ill fitting and loose dentures that move or even fall out when speaking or eating. One way of solving this problem is to construct a dental plate that goes over and attaches to something underneath it. Keeping a few natural teeth or placing dental implants in the bone under the denture also helps keep the jaw bone healthy. This avoids much of the natural jaw bone loss often seen after teeth are removed. Traditional over dentures go over natural teeth. A denture can be made that goes over and attaches to one or both cuspids. Implants supported over dentures fit on top of dental implants. A retainer bar or retention balls are placed on the implants and special attachments are inserted into the denture to grab onto these retention devices. A new method using mini implant dentures is becoming increasingly popular. Mini implants are very thin, long titanium implants that screw into the jaw bone. They can be placed and old dentures can often be retrofitted to the implant.
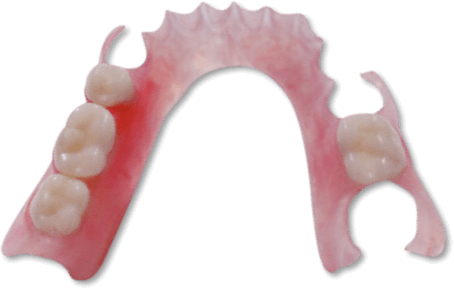
Partial Dentures are used to replace missing teeth. Partials have metal hooks that grab onto the neighboring teeth for support. Unfortunately, the hooks have a tendency to loosen up the teeth and partial dentures have the tendency to get loose and require multiple adjustments throughout the years. On the upper, there is a large piece of metal that goes across the roof of the mouth which can interfere with taste sensation and/or have food collected under it. Additionally, the partial plate can press into the gum tissue and cause sores. The partial dental plate must be taken in and out each day for cleaning. It is certainly not an ideal alternative.
Precision partial dentures are retained in the mouth by interlocking components. A specially shaped extension of the partial fits snugly into or onto a receiving area or projection of a natural tooth that has been crowned. This makes for anti-slip dentures that won't move or come out when you speak or chew.
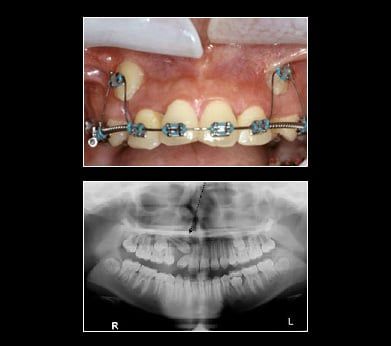
Ectopic canines are generally found in the Buccal Vestibule. Impacted canines may be retrieved with braces, using a surgical approach via a gold chain or straight wire. Tissue covering the tooth is uncovered. A chain or wire is attached to the tooth crown. Tissue is placed back over the tooth leaving the chain or wire coming out of the gum. For the purpose of this illustration a gold chain is used to retrieve the canines. The chain is attached to the tooth crown and the link is attached to a flexible archwire so that the wire is active (bent). Once a month, the wire is reactivated by using the next link up on the chain until the impacted canine erupts enough to attach a regular bracket on the canine. With the regular bracket in place, a more flexible wire is added directly to the bracketed canine. This process will bring the canine into position within the arch by forcing the canine to conform to the straight archwire form. This is a long process taking anywhere from 8-12 months.
Dr. King, an Invisalign dentist in Glen Rock, often recommends an Invisalign procedure rather than traditional braces. Invisalign is the breakthrough technology that lets you have the smile you've always wanted without the hassle of braces. By using a series of clear, removable aligners, Invisalign straightens your teeth with results you'll notice sooner than you think. The course of treatment involves changing aligners approximately every two weeks, moving your teeth into straighter position step-by-step, until you have a more beautiful smile. And unlike conventional braces, these clear aligners can be removed while you eat and brush your teeth as usual. An average Invisalign course of treatment takes about a year.
| Â | INVISALIGN | BRACES |
|---|---|---|
| Effectively treats a wide variety of cases, including crowding, spacing, crossbite, overbite and underbite. | X | X |
| Straightens your teeth | X | X |
| Average cost is about $5,000* | X | X |
| Allows you to eat whatever foods you enjoy | X | Â |
| Lets you remove the device when you want | X | Â |
| Lets you enjoy virtually invisible teeth-straightening | X | Â |
| Allows you to brush and floss your teeth normally for better periodontal health | X | Â |
| Consists of smooth, comfortable plastic instead of sharp metal that is more likely to irritate your cheeks and gums | X | Â |
| Frees up your busy schedule, with office visits only every four to six weeks | X | Â |
| Invisalign Teen: Provides up to six free replacement aligners if lost or broken.** | X | Â |
* November 2010 Invisalign Patient Survey
** Invisalign Teen Only
Research has shown that gum disease can influence heart disease and other health conditions in negative ways. They suggest that gum disease could even be a more serious factor in heart disease than smoking, cholesterol, hypertension and age. One reason for this is the fact that the bacteria found in diseased gums can come loose and move throughout the body. When this bacteria reaches arteries it can cause arterial plaque to build up and harden which in return adversely affect blood flow.

Healthy gums are generally pink and anchor the teeth firmly in place.
One of the earliest stages of gum disease is gingivitis. Gingivitis causes the gums to become swollen and bleed due to the toxins, enzymes and plaque byproducts that are created. In order for your gums to return to a healthy state, treatment from Dr. King is required in addition to proper oral hygiene.
When the bone tissue starts to deteriorate, this is known as a form of gum disease called Periodontitis. This happens when the byproducts of plaque attack the tissues that hold your teeth to the bone. The gums begin falling away from the teeth and form pockets in the gums which allows more plaque to collect below the gum line. When this occurs, the patient becomes more sensitive to hot and cold and the roots of the teeth are more vulnerable to decay.
With severe periodontitis, a radical amount of gum tissue and bone tissue is lost. Usually, teeth lose more support as the disease continues to destroy the periodontal ligament and bone. Teeth become loose and may even need to be extracted. This causes difficulties in normal everyday chewing and biting habits. If advanced periodontal disease is left untreated, patients run the risk of other serious health problems.
Teeth that are suffering damage from gum disease will always be more sensitive to cold and if you avoid cleaning them due to this sensitivity, it can only make the problem worse.
After dental treatment, some teeth may be more sensitive because this is their way of dealing with injury. Injuries to teeth such as cavities, gum infection and jaw clenching can damage the nerves in a tooth. The sensitivity should not last long after treatment as long as your teeth are kept clean, otherwise the sensitivity is likely to get worse. If your teeth are ever extra sensitive, please consult with Dr. King as this could be a sign that you need a root canal or gum tissue treatment.
Tooth loss occurs for many reasons; dental decay, root canal problems, fractures, periodontal disease and trauma. Additionally at times teeth never develop. As a result of tooth loss the bone melts away. If there is inadequate bone to support surrounding teeth and future possible dental implant(s), bone grafting materials are used to rebuild and regenerate the bone providing sufficient bone in quantity and quality for implant placements and supporting tooth structure.
Crown lengthening is a surgical procedure that re-contours the gum tissue and often the underlying bone of a tooth. Crown lengthening is often for a tooth to be fitted with a crown. It provides necessary space between the supporting bone and crown, which prevents the new crown from damaging bone and gum tissue.
When deep pockets between teeth and gums (6 millimeters or deeper) are present, it is difficult for a dentist to thoroughly remove the plaque and tartar. Flap surgery is a procedure where the gum flap is lifted away from the tooth. Diseased tissue and sometimes bone is removed. The rough surfaces of the tooth are then smoothed by root planing. The area is medicated and the gum flap is replaced and sutured allowing the bone and gum tissue to heal.
One of the goals of flap surgery is to reduce the depth of the periodontal pockets to make them easier to keep clean.
If a patient has an excess amount of tissue that connects the lower and upper lips to the jaw and gum line, a frenectomy procedure is performed to remove the excess tissue.
A gum lift may be performed to create a more even gum line. Patients with a gummy smile can quickly and safely have unwanted tissue removed, thus exposing more tooth to shape a more attractive smile.
In the back of the upper jaw bone, dental implants are frequently needed. In order for a dental implant to be successful in this area of the mouth there must be sufficient bone height and width to connect (integrate) to the dental implant. When the upper back teeth are lost and not replaced, the sinus cavity becomes enlarged destroying any bone that is left behind. This very large sinus is like a "giant air pocket" and not capable of supporting an implant. A procedure known as sinus grafting (sinus lift) is performed to create bone that will ultimately hold the implants within the sinus. Sinus grafting is an extremely common form of bone grafting.

Root exposure resulting from gingival tissue recession may pose multiple problems for patients:
- Undesirable Aesthetics
- Root Sensitivity
- Impaired Oral Hygiene
- Increased Caries Susceptibility
- Teeth May Become Loose
A gingival tissue graft will restore the proper gum tissue structure around the tooth.
Causes of a Root Canal
Root canals are necessary when a cavity that has been left untreated becomes larger. Once the cavity reaches the pulp of the tooth, an infection forms at the base of the root canal, causing an abscess. This abscess is generally painful and will need to be removed.
The doctors at Peter King, DDS know that serious tooth decay can often lead to a root canal. A root canal may be needed if the decay has reached the tooth's nerve. Essentially, a root canal involves cleaning out a tooth's infected root, then filling and sealing the canal.
Root Canal Procedure:
1) An opening is made through the crown of the tooth into the pulp chamber.
2) The pulp is removed, and the root canals are cleaned, enlarged and shaped.
3) The infected area is medicated.
4) The root canals are filled.
5) The crown opening is filled with a temporary.
If you are experiencing severe tooth pain, you may need a root canal. The only sure way to know is to call our Glen Rock, NJ dental office at 201-857-2661 and setup an appointment with Dr. King.
A post and crown is used when there is not enough tooth structure left for retention after your root canal procedure to support a crown, a post will be placed upon the tooth root. Dr. King will then make a crown buildup around the post. After that, a crown will be placed on the buildup.
If you live in the Glen Rock area and are suffering from tooth pain, call 201-857-2661 and setup an appointment to have Dr. King check your teeth and relieve your pain today. Don't suffer needlessly with tooth pain. Let the friendly staff at Peter King, DDS help you smile again.
The best material for a bone graft is your own bone, which most likely will come from your chin, the back part of your lower jaw or your hip bone. The hip is considered to be a better source because the hip bone has a lot of marrow, which contains bone-forming cells. There are also synthetic materials that can be used for bone grafting. To place the removed bone in the recipient site, little holes are drilled in the existing bone to cause bleeding. This is done because blood provides cells that help the bone heal. The block of bone that was removed will be anchored in place with titanium screws. A mixture of the patient's bone marrow and some other bone-graft material will then be placed around the edges of the bone block. Finally, a membrane is placed over the area and the incision closed. The bone graft will take about 6 to 12 months to heal before dental implants can be placed. At that time, the titanium screws used to anchor the bone block in place will be removed before the implant is placed.
Tooth loss occurs for many reasons; dental decay, root canal problems, fractures, periodontal disease and trauma. Additionally at times teeth never develop. As a result of tooth loss the bone melts away. If there is inadequate bone to support surrounding teeth and future possible dental implant(s), bone grafting materials are used to rebuild and regenerate the bone providing sufficient bone in quantity and quality for implant placements and supporting tooth structure.
Dr. King is an experienced tooth extraction dentist in Glen Rock. When the extraction of a tooth is required:
1) An incision in the gums is made
2) The tooth is removed
3) The area is stitched up and is allowed to heal
During this time, it is important to think about a tooth replacement option. An extracted tooth leaves an open area in the jaw which, in time, allows the neighboring teeth to drift into the area where the tooth was extracted. This in turn, causes a chain reaction to all the surrounding teeth. Also, if you are considering placing an implant in the future, you should consider asking your dentist to place a bone graft at the time of surgery to preserve the bone width and height.

After tooth extraction, it’s important for a blood clot to form to stop the bleeding and begin the healing process. We ask you to bite on a gauze pad in the tooth extraction area for 30 minutes after the appointment. If the bleeding or oozing persists, repeat the process. After the blood clot forms, it is important not to dislodge the clot. Do not rinse vigorously, suck on straws, smoke, drink alcohol or brush teeth next to the extraction site for 72 hours. These activities will dislodge the clot. Limit vigorous exercise for the next 24 hours as this will increase blood pressure and may cause more bleeding from the extraction site.
After the tooth is extracted you may feel some pain and experience some swelling. An ice pack applied to the area 20 minutes on, 20 minutes off, will keep swelling to a minimum. Take pain medications as prescribed by Peter King, DDS. The swelling will usually subside in about 48 hours.
Use the pain medication as directed. Call the office if the medication doesn't seem to be working. If antibiotics are prescribed, continue to take them for the indicated length of time, even if signs and symptoms of infection are gone. Drink lots of fluid and eat nutritious soft food on the day of the extraction. You can eat normally as soon as you are comfortable.
It's important to resume your normal dental routine after 24 hours. This should include brushing and flossing your teeth at least twice a day. This will speed healing and help keep your mouth fresh and clean.
After a few days you will feel fine and can resume your normal activities. If you have heavy bleeding, severe pain, continued swelling after 2-3 days, or a reaction to the medication, call our office immediately at 201-857-2661.
After the Removal of Multiple Teeth
BLEEDING. A small amount of bleeding is to be expected following the operation. If bleeding occurs, place a gauze pad directly over the bleeding socket and apply biting pressure for 30 minutes. If bleeding continues, a moist tea bag can be used for 30 minutes. If bleeding occurs, avoid hot liquids, exercise, and elevate the head. If bleeding persists, call our office immediately. Do not remove immediate denture unless the bleeding is severe. Expect some oozing around the side of the denture.
SWELLING. Use ice packs on the same side of the face of the surgical area. Apply ice 20 minutes on, 20 minutes off, during your waking hours for a maximum of 36 hours only. Ice does not have an effect after 36 hours. Call the office for further assistance.
DISCOMFORT. For mild discomfort use aspirin, Tylenol or any similar medication; two tablets every 3-4 hours. Ibuprofen (Advil, Motrin) 200mg can be taken 2-3 tablets every 3-4 hours. For severe pain use the prescription given to you. If the pain does not begin to subside in 2 days, or increases after 2 days, please call our office. If an antibiotic has been prescribed, finish your prescription regardless of your symptoms.
DIET. Drink plenty of fluids. If many teeth have been extracted, the blood lost at this time needs to be replaced. Drink at least six glasses of liquid the first day. Restrict your diet to liquids and soft foods, which are comfortable for you to eat. As the wounds heal, you will be able to advance your diet.
HOME HYGIENE CARE. Do not rinse your mouth for the first post-operative day, or while there is bleeding. After the first day, use a warm salt water rinse every 4 hours and following meals to flush out particles of food and debris that may lodge in the operated area. (One half teaspoon of salt in a glass of lukewarm water.). After you have seen your dentist for denture adjustment, take out denture and rinse 3 to 4 times a day.
WEARING DENTURES. The removal of many teeth at one time is quite different than the extraction of one or two teeth. Because the bone must be shaped and smoothed prior to the insertion of a denture, the following conditions may occur, all of which are considered normal:
- The area operated on will swell reaching a maximum in two days. Swelling and discoloration around the eye may occur. The application of a moist warm towel will help eliminate the discoloration quicker. The towel should be applied continuously for as long as tolerable beginning 36 hours after surgery (remember ice packs are used for the first 36 hours only).
- A sore throat may develop. The muscles of the throat are near the extraction sites. Swelling into the throat muscles can cause pain. This is normal and should subside in 2-3 days.
- If the corners of the mouth are stretched, they may dry out and crack. Your lips should be kept moist with an ointment like Vaseline. There may be a slight elevation of temperature for 24-48 hours. If temperature continues, notify our office.
If immediate dentures have been inserted, sore spots may develop. In most cases, Peter King, DDS will see you within 24-48 hours after surgery and make the necessary adjustments to relieve those sore spots. Failure to do so may result in severe denture sores, which may prolong the healing process.

Fold a piece of clean gauze into a pad thick enough to bite on and place directly on the extraction site. Apply moderate pressure by closing the teeth firmly over the pad. Maintain this pressure for about 30 minutes. If the pad becomes soaked, replace it with a clean one as necessary. Do not suck on the extraction site (as with a straw). A slight amount of blood may leak at the extraction site until a clot forms. However, if heavy bleeding continues, call your dentist. (Remember, though, that a lot of saliva and a little blood can look like a lot of bleeding).
The Blood Clot
After an extraction, a blood clot forms in the tooth socket. This clot is an important part of the normal healing process. You should therefore avoid activities that might disturb the clot.
Here's how to protect it:
- Do not smoke, rinse your mouth vigorously or drink through a straw for 24 hours.
- Do not clean the teeth next to the healing tooth socket for the rest of the day. You should, however, brush and floss your other teeth thoroughly, gently rinse your mouth afterwards.
- Limit strenuous activity for 24 hours after the extraction. This will reduce bleeding and help the blood clot to form. Get plenty of rest.
- If you have sutures, your dentist will instruct you when to return to have them removed.
Medication
Your dentist may prescribe medication to control pain and prevent infection. Use it only as directed. If the medication prescribed does not seem to work for you, do not increase the dosage. Please call your dentist immediately if you have prolonged or severe pain, swelling, bleeding, or fever.
Swelling & Pain
After a tooth is removed, you may have some discomfort and notice some swelling. You can help reduce swelling and pain by applying cold compresses to the face. An ice bag or cold, moist cloth can be used periodically. Ice should be used only for the first day. Apply heat tomorrow if needed. Be sure to follow your doctor's instructions.
Diet
After the extraction, drink lots of liquids and eat soft, nutritious foods. Avoid alcoholic beverages and hot liquids. Begin eating solid foods the next day or as soon as you can chew comfortably. For about two days, try to chew food on the side opposite the extraction site. If you are troubled by nausea and vomiting call your dentist for advice.
Rinsing
The day after the extraction, gently rinse your mouth with warm salt water (teaspoon of salt in an 8 oz. glass of warm water). Rinsing after meals is important to keep food particles away from the extraction site. Do not rinse vigorously!
Do you ever experience a clicking or popping sound when opening or closing your mouth? Have you been suffering from headaches or migraines and no one seems to be able to help you? Have you been taking pain medicine for years and would like to get off of it? Do you feel any clogging or congestion in one or both of your ears? These are just a few of many symptoms that might be associated with TMD, or Temporomandibular Dysfunction, a common condition affecting the jaw joint or Temporomandibular Joint (TMJ).
TMJ dysfunction, often referred to as TMD, is a disharmony between the way the jaw joint works in an unstrained position and the way the teeth and bite work during those movements. Possible causes of this disharmony include tooth loss, accidents (like whiplash), mal-positioned and/or underdeveloped cranial or jawbones, and perhaps habits like clenching or teeth grinding. Many people go through life suffering from headaches and a variety of facial and neck pains without knowing the ultimate cause, which in many cases is TMJ disorder.
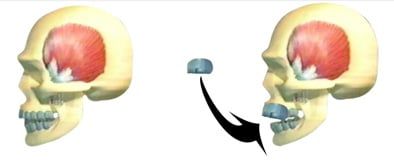
They are the two joints which connect the lower jaw to the temporal bone at the side of the head. If you place your fingers just in front of your ears and open your mouth, you can feel the joint on each side of the head. Because these joints are flexible, the jaw can move smoothly up and down and side to side, enabling us to talk, chew and yawn. When the TMJ is not functioning normally and it is not within its physiological limits, it creates a condition called TMD, or Temporomandibular Dysfunction.
TMD is a group of conditions resulting from not having a normal function or "comfortable" positioning of the TMJ, and will present as a cycle of pain, muscle spasms and jaw problems. When teeth are missing, out of alignment, crowded or misshaped, chewing and biting cannot be achieved in a balanced way, so the TMJ and the muscles of chewing try to compensate for this unbalanced movement which results in symptoms that will confirm the presence of TMD.
Temporomandibular Joint Disorder (TMD) is not just a disorder, but a group of conditions, often painful, that affect the jaw joint or Temporomandibular Joint (TMJ) and the muscles that control chewing.
When teeth are missing, or out of alignment, it causes the jaw to shift positions and the muscles to work harder to chew, swallow, bite...etc and eventually will cause: muscle spasms, tension and pain.
Muscle tension and misplaced TMJ could cause the TMJ disc to be pulled out of place which will result in pain, clicking and popping in the TMJ.
If the disc is displaced for a long time, the bones will start rubbing against each other and some damage will happen to the bone, this is called Osteoorthrosis.
If there is inflammation in other joints or bones of the body, it is called Osteoarthritis (Arthritis) which may involve the jaw bone and the TMJ. Some damage to the bone may be evident on the x-rays.
While recognizing TMJ problems is within the ability of most physicians and dentists, not all practitioners are qualified to diagnose it properly and treat it right. It is imperative that a trained practitioner in Craniofacial pain or Neuromuscular Dentistry give the final and definitive diagnosis, and suggest the most suitable treatment plan.
There is a lot of skepticism about TMJ treatment in the medical society and that is simply due to the fact that physicians didn't receive the dental training and didn't acquire the knowledge required for such complicated diagnosis and treatment. Furthermore, many dentists rush into treating TMJ thinking that they can cure these problems, only to find that they lack the skill and experience to get the job done.
We have training and experience in the treatment of these problems with outstanding success rates. With highly advanced equipment and a high level of knowledge, we address your concerns and provide the best diagnosis for the optimal treatment.
Many patients who suffer from TMD symptoms, were never told that it is related to their TMJ problem and were not aware that treating their TMJ could easily relieve their suffering. To explain this further...
If you suffer from headaches or migraines, TMJ dysfunction, could be the major and most likely cause of your suffering. Your doctors, including neurologists, have simply not received the dental training required to relate your migraine or headache pain to your TMJ problems. Once you rule out any brain tumors or aneurysms, TMJ should be checked and TMD should be treated to relieve the headaches and migraines.
Due to the proximity of TMJ to the ears, it is very common for the ears to feel congestion, or to have ringing in the ears when the TMJ bones move or dislocate from their place. In this case, ENT's (ear doctors) won't find anything wrong with the ears, yet the patients keep complaining about their ears. Once the TMJ is put back into its natural position, the pressure put on the ears will be relieved and the congestion disappears.
When the TMJ is not in a balanced position, it affects the general posture of the body. When the posture is not straight and upright, the nerves coming out from the spine could be irritated, which could cause the numbness or tingling feeling in the fingertips.
We use a state-of-the-art jaw tracking system that helps diagnose TMJ Dysfunction (TMD) by tracking the jaw movement. Research shows that there are certain jaw movements which show very specific types of TMJ dysfunction. For example, limited opening and closing or locking, jaw opening deviations and deflections, and restricted side-to-side jaw movements. All of these indications are widely accepted and published criteria for diagnosing TMD.
The Joint Vibration Analysis (or JVA) has been accepted by the American Dental Association to help provide a fast, non-invasive method to accurately diagnose TMJ function and demonstrate the severity level of the problem.
We use an Electromyographic Analysis (or EMG) to measure muscle activity on head and neck muscles both at rest and in function. This is done by placing computerized sensors on the skin allowing us to accurately monitor muscle activity. Hyperactive muscles are common for patients experiencing pain symptoms associated with TMJ problems. Imbalances between right and left sides of the same sets of muscles are also typical. The EMG system is a safe and comfortable method do help detect such issues and getting to the root of a TMJ issue.
TMJ/TMD is treatable most of the time. Simple cases of TMJ can be treated with anti-inflammatory medications and a hot/moist compress.
Generally speaking, it includes the fabrication of an orthotic. An orthotic is an acrylic device that is worn on the lower teeth 24 hours a day. The orthotic is designed to reposition the jaw to the correct neuromuscular position. We analyze the bite, decide which muscles are causing the pain, and where the current position of the bone is and the disc. All this is done with the aid of advanced equipment like the TENS unit, K7 jaw tracking, Sonography, EMG's and advanced x-rays like Tomography, CT Scans and MRI's of the TMJ. This will help us determine the best and most comfortable position of the TMJ and the muscles. Once that position is determined, we place the orthotic on the lower teeth to keep the TMJ in that position. Orthotics usually are worn for 4-6 months or until most of the symptoms are relieved. Once an orthotic is in use, the symptoms start gradually disappearing until we reach a point that both the doctor and the patient are satisfied with. This concludes Phase I of the treatment.
After 4-6 months of relief and when the patient is no longer suffering from any TMD symptoms, Phase II will be considered. Phase II includes any of the following:
Most of the time, any of the above could be considered and chosen, depending on the patients' preferences and financial capability. If you are currently suffering from TMD, it is too early to think of phase II at this time, since it is important to get you out of your pain and symptoms.
Many patients complain that when they received dentures, they noticed pain in the jaw, headaches, ear problems and other symptoms. Sometimes taking the dentures out will relieve those symptoms. If your dentures are not made to the correct bite, or vertical dimension, it will most likely cause these symptoms. Simple adjustments could get rid of these symptoms, but sometimes a whole new set of dentures need to be made according to the neuromuscular principles, to rid you of your headaches or jaw pain.
An orthotic is an acrylic device that is worn on the lower teeth 24 hours a day. It is designed to reposition the jaw to the correct neuromuscular position.
An orthotic, sometimes called a Bite Splint, is a very effective method in relieving TMD symptoms. It provides an acrylic platform to bite against, sometimes moving the mandible to a new position that is more comfortable.
An orthotic, sometimes called a Bite Splint, is a very effective method in relieving TMD symptoms. It provides an acrylic platform to bite against, sometimes moving the mandible to a new position that is more comfortable.
It can be worn on the lower teeth 24 hours a day and is designed to re-position the jaw to the correct neuromuscular position.
The NTI-TSS System is a type of mouth guard that is placed on the patient's upper teeth. This lets the lower jaw rest in its proper place and causes the teeth to subside from being able to clench together.
If you experience chronic headaches, please ask your doctor because the NTI-TSS System could work for you.
Dr. King works with sleep apnea dental patients in the Glen Rock area. Obstructive Sleep Apnea is very common and if left untreated can cause individuals to stop breathing during their sleep for a minute or more. Each time this happens the brain will wake a person up for a moment in order to get them breathing again, which results in sleep being interrupted frequently and leaving the individual tired throughout the day.
Obstructive Sleep Apnea
If your bed partner notices that you snore or gasp for air regularly while sleeping, you may have Obstructive Sleep Apnea (OSA). Not everyone who snores has OSA, however everyone who has OSA does snore. OSA is a condition in which people stop breathing for short periods, several times if not hundreds of times per night. Sleep apnea effects 13-17% of all adult Americans. Undetected sleep apnea is serious and can lead to obesity, diabetes, high blood pressure, heart attack, stroke and even death. Sever Obstructive Sleep Apnea can take 10 to 15 years off one's life.
Obstructive Sleep Apnea Causes
Obstructive Sleep Apnea is caused by a blockage of the upper airway. It may be related to the tongue being too small, muscle weakness around the throat, or fat around the airway caused by excessive weight gain which leads to the collapse of the airway during sleep. Waking up activates the body's fight-or flight response causing increased heart rate, heart stress and high blood pressure.
Obstructive Sleep Apnea Symptoms
- If you are told by your bed partner that you snore or gasp for air during your sleep.
- If you are tired and un-rested after sleep and need to take frequent naps.
- If you have hard-to-treat blood pressure.
- If you are obese and/or have a collar size larger than 16 inches for women or 17 inches for men.
- If you wake up with a dry or sore throat.
- If you are irritable in the morning or have morning headaches.
- If your legs feel twitchy at night.
Obstructive Sleep Apnea Diagnosis
OSA can only be properly diagnosed by a board-certified M.D. in sleep medicine. This is done either through spending a night in a sleep lab connected to wires and monitors or by a home sleep test. In our office, we have home sleep testing monitors which you can wear to bed in your own home. When you bring the testing unit back to our office, we will upload the data stored in the unit to a board-certified sleep physician who will diagnose if you have sleep apnea. The physician will also determine how severe the sleep apnea is and prescribe what treatment options would be appropriate. Treatment options include dental, medical or surgical.
Obstructive Sleep Apnea Treatment Alternatives
Until recently, the recommended solution was to pump air into the blocked passage by the use of a Continuous Positive Airway Pressure (CPAP) machine. It's appearance has been described like being a bulky jet pilots mask to something resembling a Darth Vader's mask. It's cumbersome, noisy and uncomfortable, but it will keep you alive. The problem is that most people use the mask on an inconsistent basis, which provides only limited value and still puts the patient at risk. Recent advancement in a specialized custom dental fabricated mouth guard provides a more comfortable solution. This small mouthpiece that rests inside the sleeper's mouth moves the jaw forward creating suction to open the throats airway. Research hasn't yet proven that treatment can reverse Obstructive Sleep Apnea, but does decrease or eliminate many of the bad outcomes.
A snoring appliance is a custom fit mouthpiece that is made from plastic and is easy to clean with a toothbrush. It is designed to keep the upper and lower jaw in place when the throat relaxes during sleep. This allows the air passage to remain open while providing a quiet and relaxing sleep.
Snoring is caused when the muscles and soft tissue in the throat and mouth relax making the breathing airway smaller. A relaxed and/or collapsed airway produces soft tissue vibrations during breathing and snoring is the result.
An oral appliance can greatly reduce or stop snoring for most people.